Patient case #7 - Borrelia hermsii infection
Description
A ten-year-old girl who recently returned from a camping trip near Lake Tahoe, Nevada, was seen in the urgent care center with fever, headache, nausea and vomiting. A viral infection was suspected and she was sent home. A few days later the child was brought to the hospital with tachycardia, rapid shallow breathing, abdominal tenderness, and hypotension. She appeared toxic on physical exam. Initial testing showed an elevated lactic acid level and acidosis (abnormal blood gases). She was immediately transferred to the ICU in septic shock, requiring emergency intubation and extracorporeal membrane oxygenation (ECMO).
Additional testing included CBC and diff:
| WBC | 15.6 x 109/L |
| Hemoglobin | 9.8 g/dL |
| MCV | 87.0 fL |
| Platelets | 15 x 109/L |
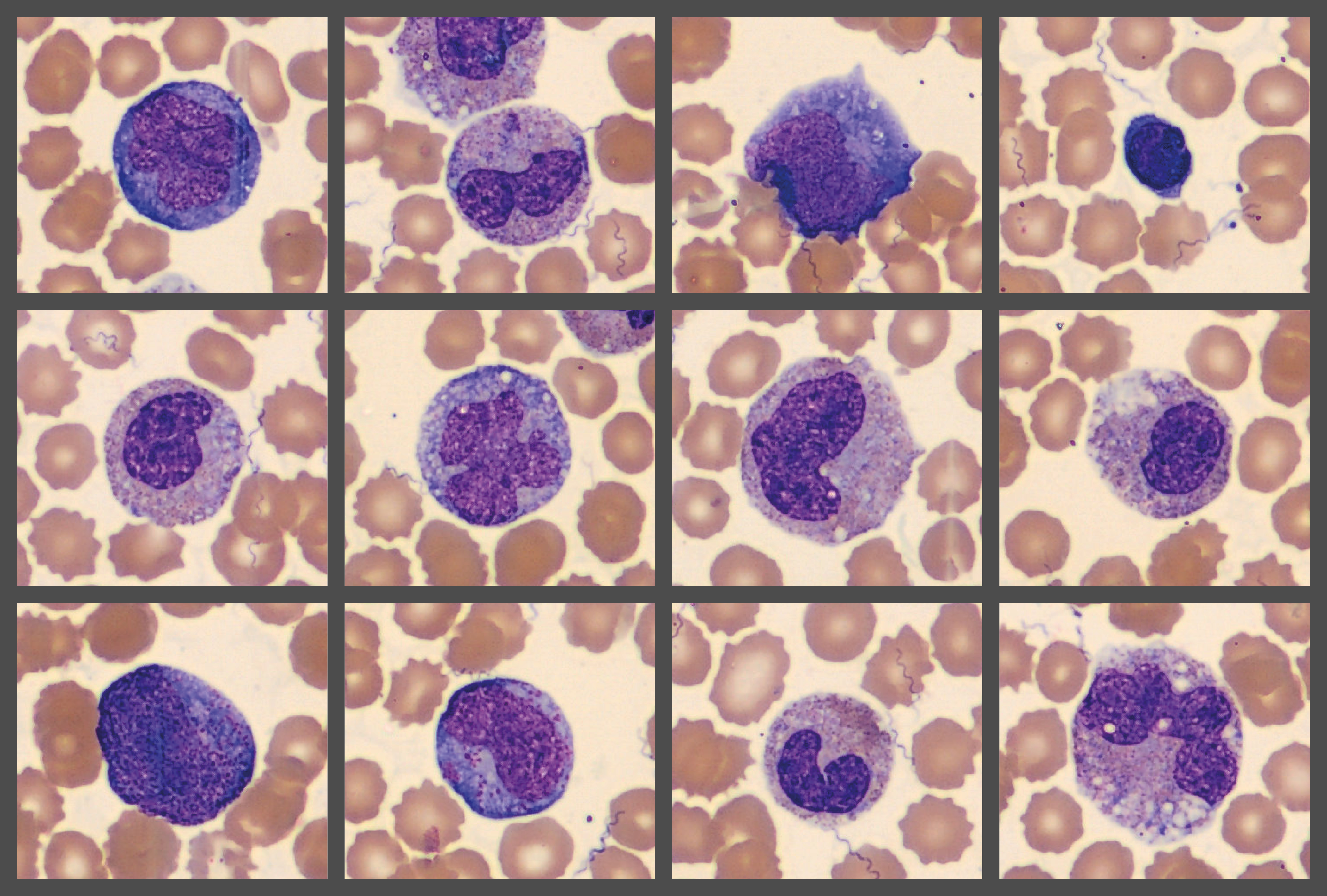
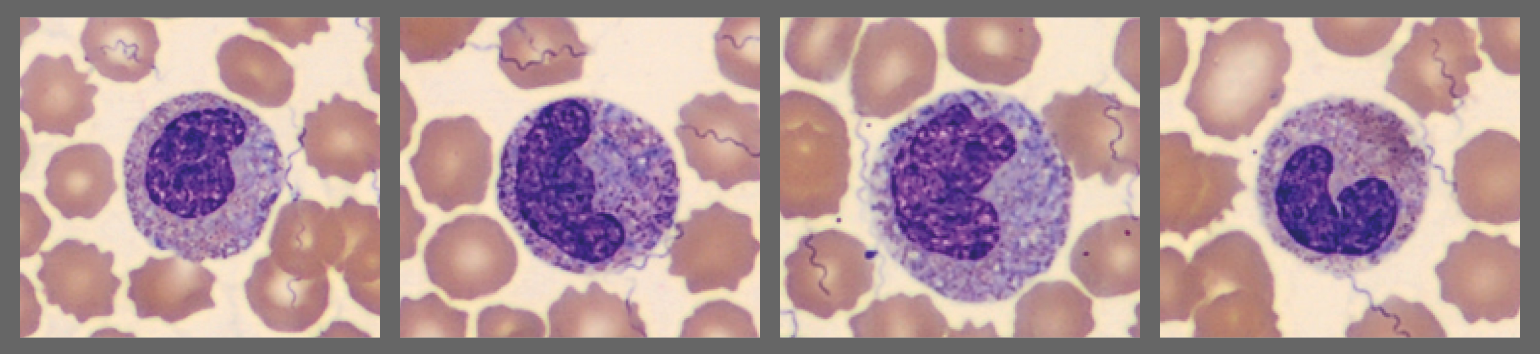
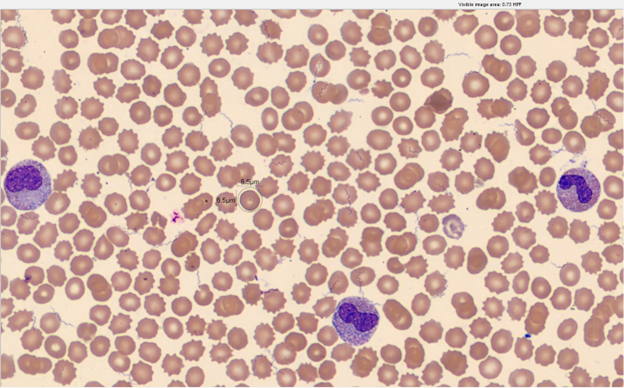
Multiple flags triggered a blood smear review on Cellavision DC-1.
|
(%) |
|
| Neutrophils |
81 |
| Lymphocytes |
10 |
| Monocytes |
5 |
| Metamyelocytes |
2 |
| Myelocytes |
1 |
| Promyelocytes |
1 |
While reviewing preclassification results, the clinical lab scientist found spirochete organisms.
The clinical team was notified of this finding and the patient was started on IV penicillin, meropenem, and doxycycline. She slowly recovered and was eventually discharged from the hospital.
Blood cultures were negative. A sample was sent for microbial cell-free DNA (cfDNA) next-generation sequencing (Karius Test) which identified Borrelia hermsii.
Diagnosis/Summary
Septic shock associated with Borrelia hermsii infection.
Borrelia hermsii is the primary cause of tick-borne relapsing fever (TBRF) in western North America. It is a rodent associated spirochete bacteria transmitted by the fast-feeding tick Ornithodoros hermsii. Infected patients are rarely aware of having been bitten. Septic shock has not been previously reported in patients with Borrelia hermsii infection.
Microscopic examination of peripheral blood smears remains an important test for identifying infected patients. The clinical lab scientist’s recognition of spirochetes while reviewing images on Cellavision enabled quick initiation of antibiotic therapy in this critically ill child.