Monthly Cell Challenge #8 / 2025
Hidden in the Smear!
Description:
A 7-year-old spayed female German Shepard came to the vet clinic after the owners noticed a few days of reduced general condition, fatigue, loss of appetite and labored breathing. The veterinarian ordered a CBC and differential.
CBC results:
| Test | Result | Units | |
|---|---|---|---|
| WBC | 4,3 | x109/L | (Ref: 5.05–16.76 x109/L |
| HCT | 0,21 | L/L | (Ref: 0.373–0.617 L/L) |
| PLT | 2 | x109/L | (Ref: 148–484 x109/L) |
| RETICS | 14.2 | K/µl | (Ref: 10.0–110.0 K/µl) |
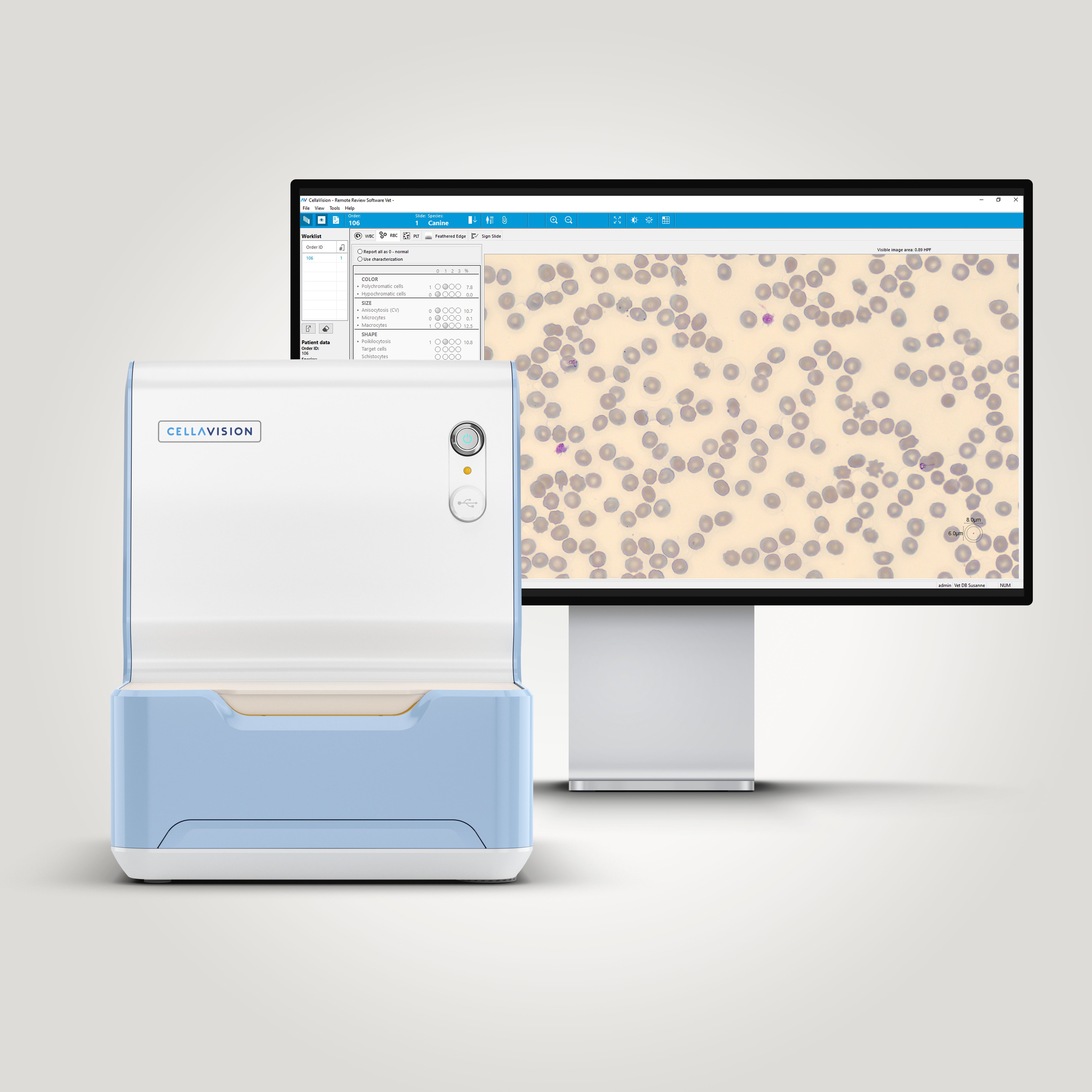
Smear review on CellaVision® DC-1 VET Remote review
| WBC Differential | % | x109/L | |
|---|---|---|---|
| Neutrophils | 86,4 | 3,7 | (Ref: 2.96–11.64 x109/L) |
| Lymphocytes | 5,5 | 0,2 | (Ref: 1.05–5.10 x109/L) |
| Monocytes | 8,0 | 0,3 | (Ref: 0.16–1.12 x109/L) |
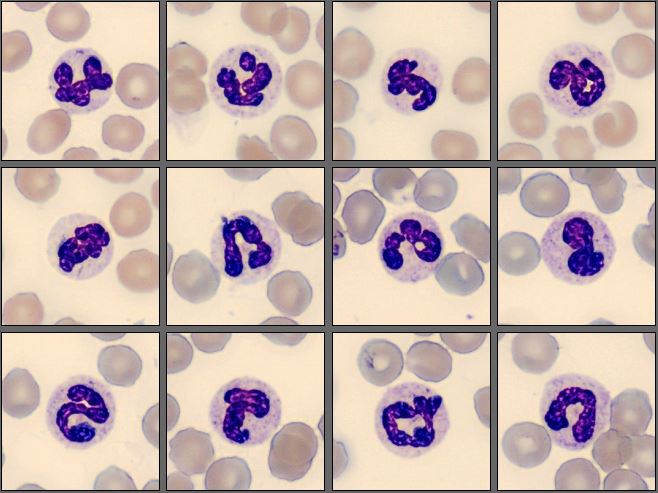
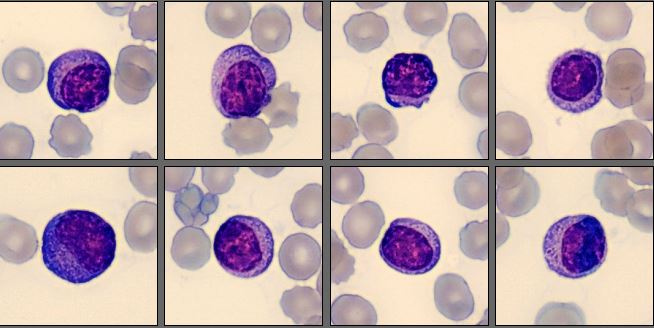
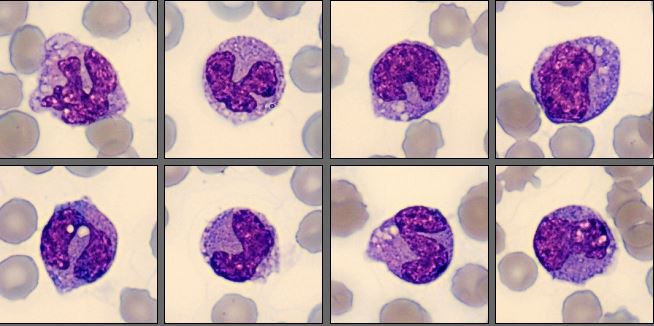
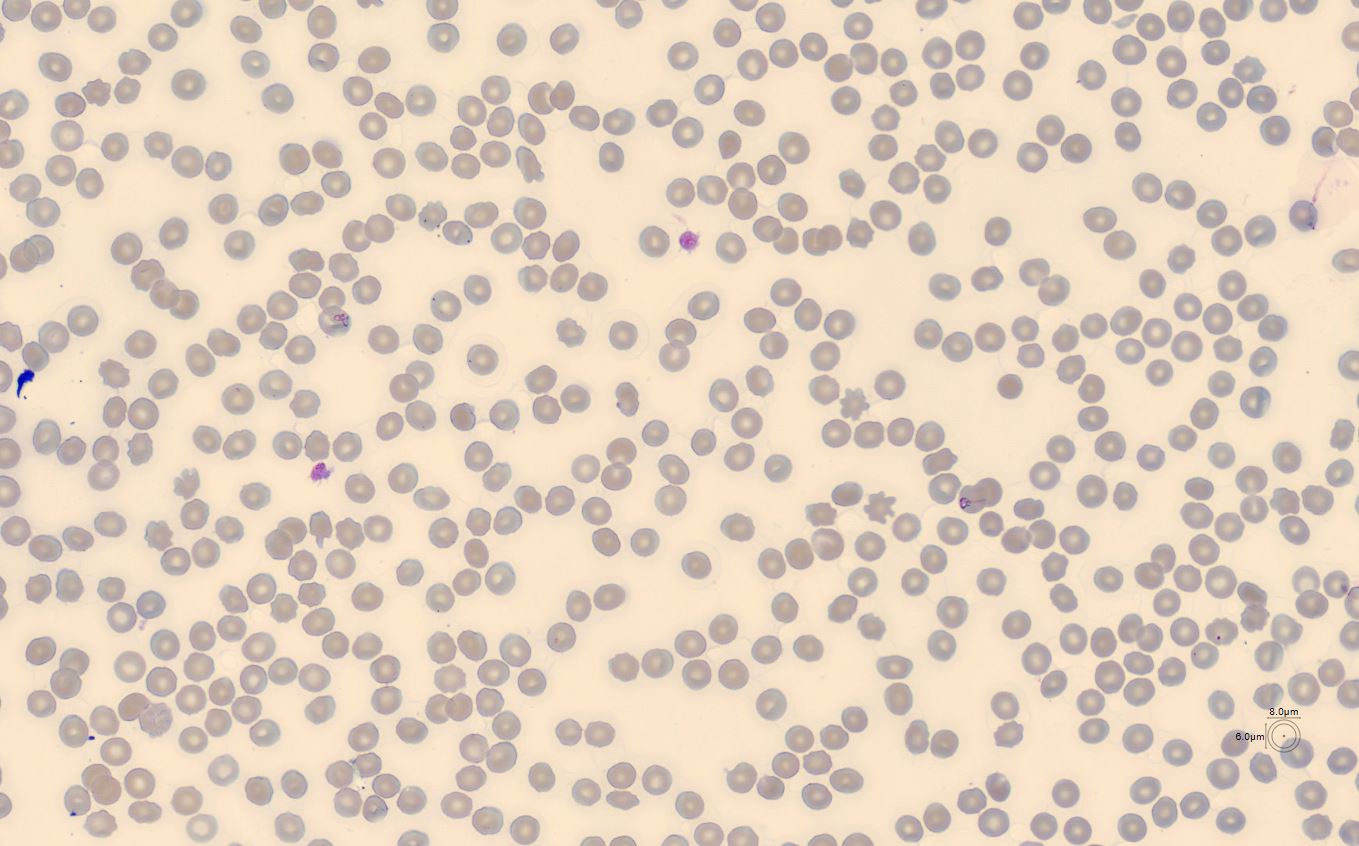
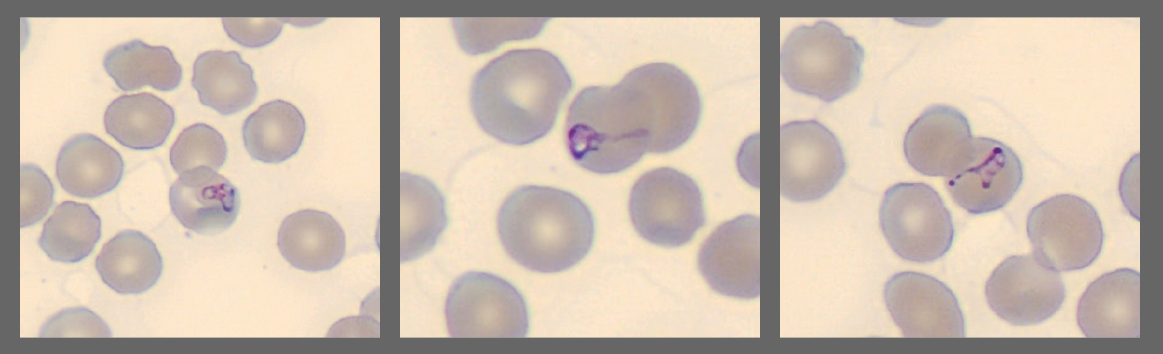
The WBC morphology looked normal,with some anemia, leukopenia and lymphopenia. There was also a marked thrombocytopenia. While the MedTech went through the differetial, there was someting supicious in the edge of one of the neutrophil images. When shifting to the RBC view they noticed something that should not be there.
Diagnosis:
Babesiosis
Discussion:
Babesia is a tick-borne infection, caused by the Babesia protozoal parasite. It invades mammalian red blood cells after a tick bite and will cause anemia. The infection can also cause a low platelet count due to a trigger from the parasite which activates an immune response that damages the platelets. The parasite can also infect and destroy the platelets directly. Animals with or without clinical signs can spread the infection either to a new tick or by exposure to infected blood or even dog-to-dog contact, for example if they bite each other.[1][2][3]
The Babesia protozoa is found across the world, and there are more than 100 different species of Babesia. It can infect a wide range of animals, both wild and domestic, for example cattle, horses, sheep, cats, dogs, deer, lions, primates, and occasionally humans. [4]
There are multiple different types of ticks which can spread the infection and the tick must bite, attach and feed from the dog for about 2-3 days. The incubation time varies, but on average, symptoms usually start 2 weeks after exposure. Some cases are not diagnosed until months or even years after the exposure. [2]
Symptoms can vary from mild to severe and can even result in death. Some symptoms are lethargy, depression, loss of appetite, fever, enlarged lymph nodes, enlarged spleen, jaundice, and neurological signs like imbalance, seizures and neck pain. [1][2]
Babesiosis is often discovered incidentally when the owners bring their dog to the veterinarian due to reduced general condition and with one or more of the symptoms mentioned above. [2]
The symptoms of Babesiosis can easily be confused with other illnesses. Some of the tests that can be used to discover the babesia infection is:
• Blood cell differential with a Romanowsky stain, which allows for the parasite to be seen in the red blood cells.
• Immunofluorescent antibody test to look for antibodies in the blood serum.
• ELISA test which is dependent on the antibody response by the infected animal.
• PCR test to look for Babesia DNA in the infected animal.[1][2]
Treatment depends on the protozoa species and how affected the dog is from the infection. First, there are antiprotozoal medication to eliminate the parasite from the blood stream. If the dog is anemic, a blood transfusion could be needed. And if the dog is severely affected, further support such as oxygen, IV-fluid, steroid medication, anti-inflammatory, and anti-nausea medication could be necessary. [2][5]
References:
[1] Weir. M, et.al., Babesiosis in Dogs, (2022) LifeLearn Inc, https://vcahospitals.com/know-your-pet/babesiosis-in-dogs (accessed: 2025-06-16)
[2] Morrison. B.J., Babesiosis in Dogs, (2022), https://www.petmd.com/dog/conditions/infectious-parasitic/c_dg_babesiosis (Accessed: 2025-06-16)
[3] Narurkar. R et.al., Babesiosis-associated immune thrombocytopenia, (2017). (Accessed: 2025-06-16)
[4] Carter. P.D. et.al., Babesiosis in Animals, (2022), https://www.msdvetmanual.com/circulatory-system/blood-parasites/babesiosis-in-animals (Accessed: 2025-06-16)
[5] Wag!, Babesiosis in dogs, https://wagwalking.com/condition/babesiosis (Accessed: 2025-06-16)