Patient case #2 - Anaplasmosis

Description
A 45-year-old man presented to his medical practitioner with recent onset of fever, chills, weakness, and muscle soreness. Routine laboratory tests were performed.
Results:
| WBC | 4.4 x 109/L |
| Hemoglobin | 9.3 g/dL |
| MCV | 101.3 fL |
| Platelets | 51 x 109/L |
| Creatinine | 2.1 mg/dL |
| AST | 92 U/L |
| ALT | 115 U/L |
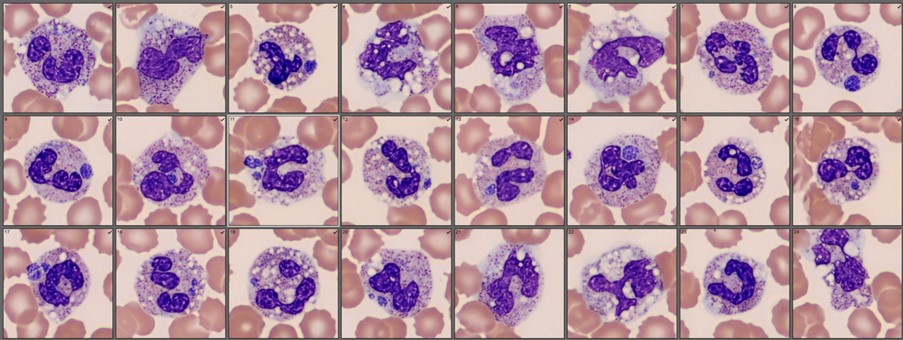
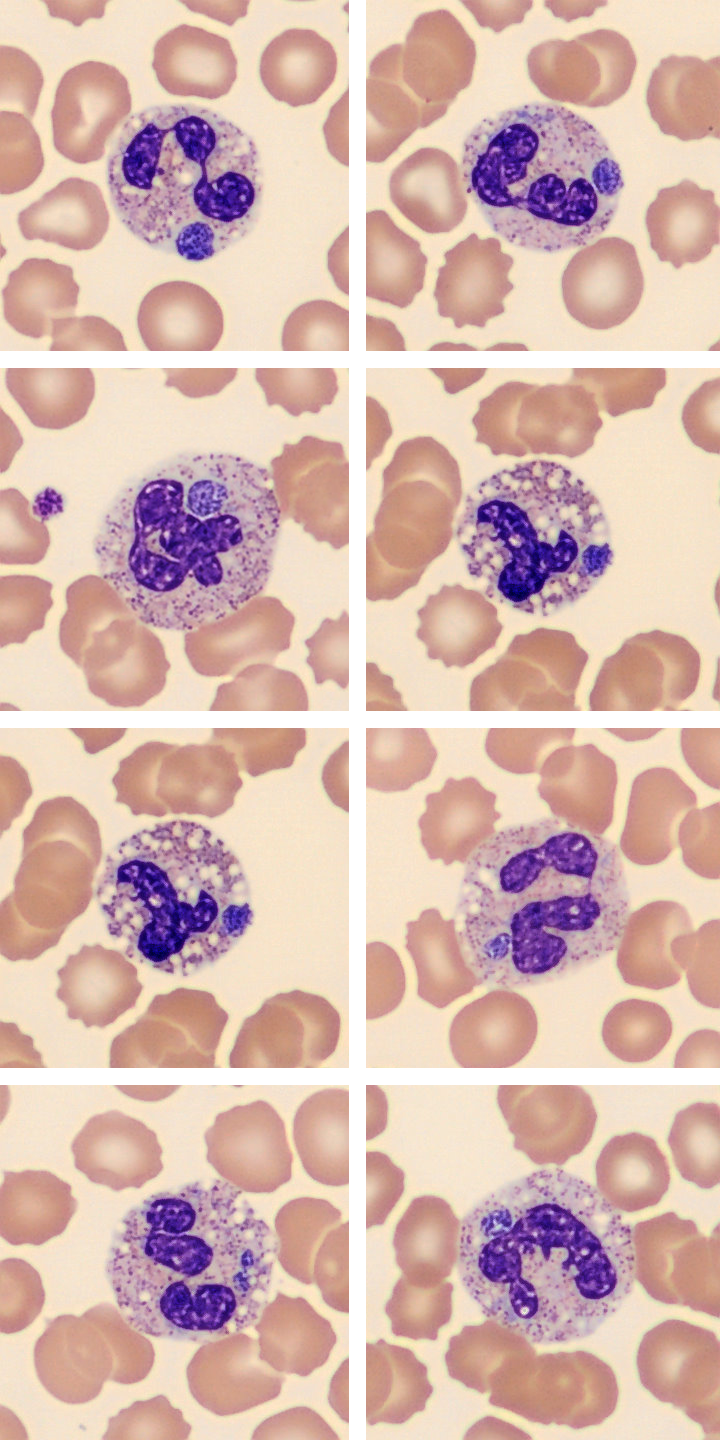
A low platelet count triggered a blood film review on Cellavision DC-1. There were 96% neutrophils with marked vacuolation, slight toxic granulation and few Dohle bodies. Approximately 30% of these cells contained 1-2 circular basophilic inclusions of variable size. At higher magnification, the inclusions were found to be morulae, composed of aggregates of coccoid bacteria [image 2]. Based on these findings, the patient was treated with doxycycline and showed noticeable improvement on the third day. Polymerase chain reaction (PCR) testing later identified the organism Anaplasma phagocytophilum and the patient was subsequently diagnosed with human granulocyte anaplasmosis (HGA).
Summary/Diagnosis
HGA is a tick-borne bacterial infection caused by Anaplasma phagocytophilum that has been reported throughout the world. While the disease is often self-limiting, nearly a third of patients develop more severe disease requiring hospitalization. The fatality rate of HGA is approximately 1%.1 Quick recognition and early antibiotic (doxycycline) treatment are key in reducing associated complications.
Polymerase chain reaction (PCR) and serological tests are commonly used to confirm HGA diagnosis, however they can be time consuming, costly, and sometimes unavailable, especially in resource limited areas. Rapid diagnostic tests for HGA have not been developed for widespread use. Treatment is recommended on the basis of clinical suspicion.2
A microscopic examination of the blood film represents a quick and cost effective test in early stage HGA as up to 80% of patients exhibit intracellular morulae.3 Using digital morphology, it is possible to simultaneously screen the entire population of neutrophils which can assist in morulae detection and help identify HGA patients in need of antibiotic therapy.
___
1. Dahlgren, F. S., Mandel, E. J., Krebs, J. W., et al. (2011). Increasing incidence of Ehrlichia chaffeensis and Anaplasma phagocytophilum in the United States, 2000-2007. Am J Trop Med Hyg, 85(1), 124-131.
2. Bakken, J. S., Krueth, J., Wilson-Nordskog, C., et al. (1996). Clinical and laboratory characteristics of human granulocytic ehrlichiosis. JAMA, 275(3), 199-205.
3. CDC. (2019). Anaplasmosis. Washington DC: Centers for Disease Control and Prevention.