Monthly Cell Challenge #12 / 2025
A Granular Mystery in the Peripheral Blood
A 3-year-old boy was referred for hematologic evaluation due to unusual granulation observed in his white blood cells on a recent peripheral smear. His parents reported frequent respiratory infections, progressive joint stiffness, and mild developmental delay. On examination, he appeared short in stature with coarse facial features and mild hepatosplenomegaly.
CBC results:
| Test | Result | Units |
|---|---|---|
| WBC | 7,95 | x109/L |
| HGB | 113 | g/L |
| MCV | 82,4 | fL |
| PLT | 227 | x109/L |
A complete blood count revealed normal white blood cells and platelet counts with mild anemia. The automated hematology analyzer flagged “WBC Abn Scattergram” and “Blast/Abn Lympho?”, prompting a manual differential and peripheral blood smear review. The blood smear was stained with May-Grünwald Giemsa and analyzed using the CellaVision® DC-1.
Smear review on CellaVision® DC-1
| WBC Differential | % | x109/L |
|---|---|---|
| Neutrophils | 83,3 | 6,7 |
| Basophils | 2,4 | 0,2 |
| Lymphocytes | 12,4 | 1,0 |
| Monocytes | 1,9 | 0,2 |
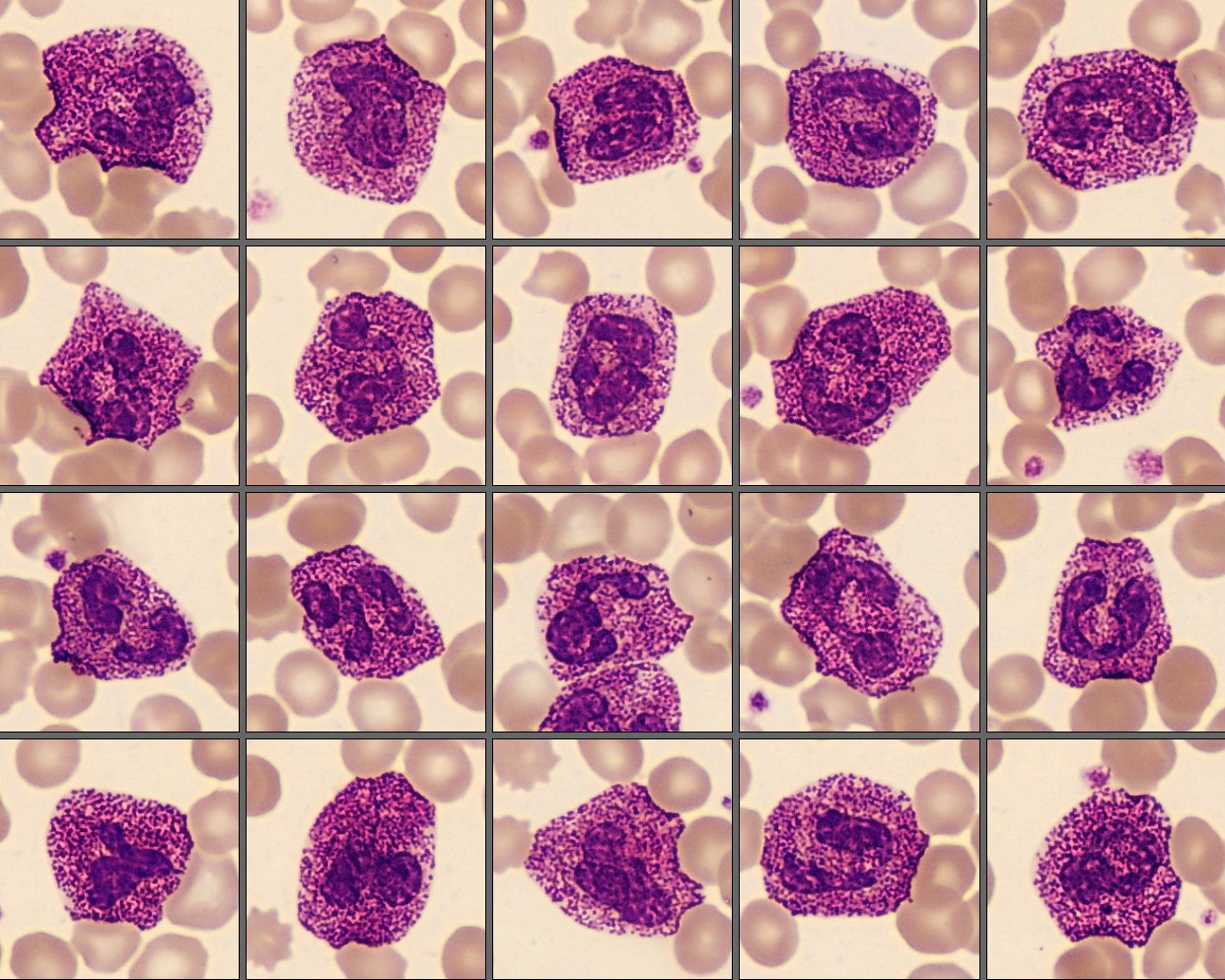
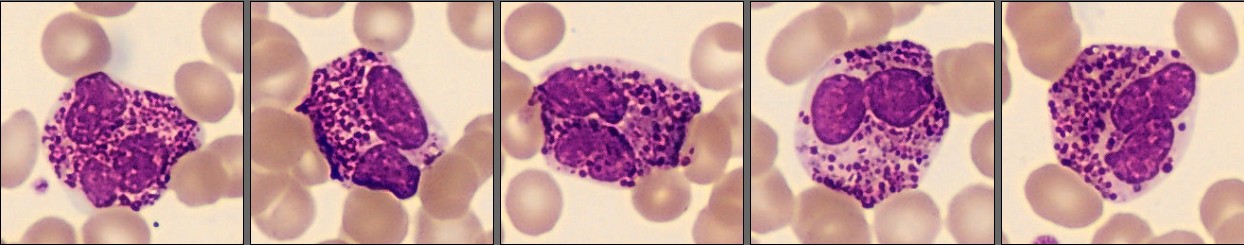
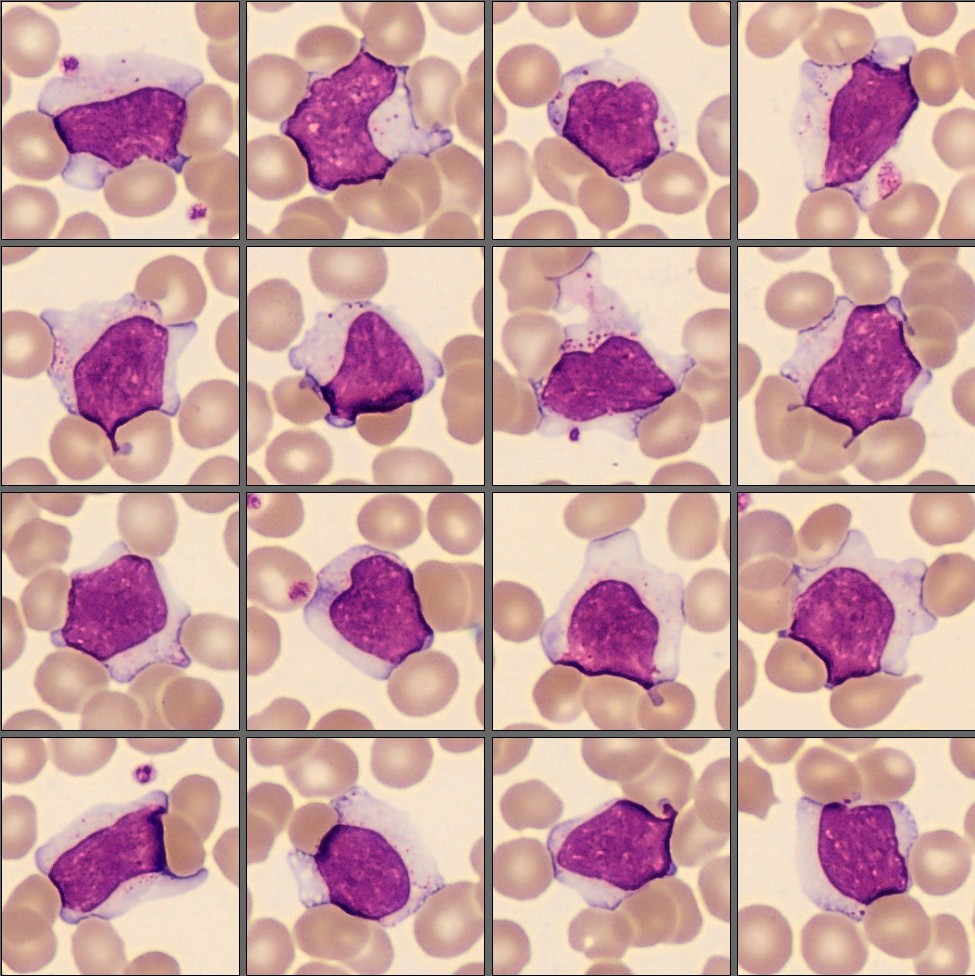
On the CellaVision® Remote Review Software, the leukocytes appeared morphologically mature, but many showed strikingly coarse, dark-purple cytoplasmic granules distributed throughout the cytoplasm. The granulation was present not only in neutrophils but also in occasional lymphocytes and monocytes. No left shift, Döhle bodies, or toxic changes were noted. Red cell and platelet morphology were unremarkable.
Diagnosis:
Alder–Reilly anomaly
Discussion:
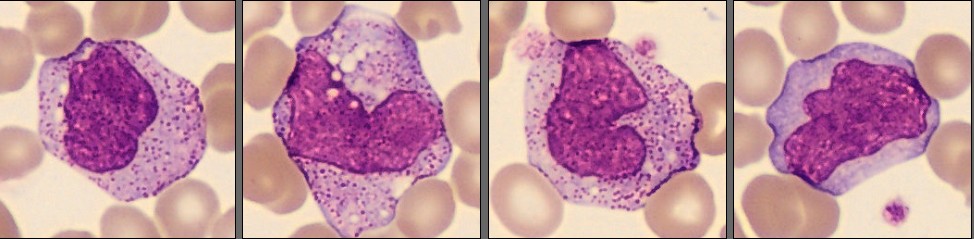
The peripheral blood smear shows mature white blood cells with coarse, dense, dark-purple cytoplasmic granules when stained with May-Grünwald Giemsa. The granules vary in size and are generally larger and more refractile than normal specific granules. In some cells, they partially obscure the cytoplasm and give it a slightly metachromatic tone. The nuclei are normally segmented, and there is no left shift, vacuolization, or presence of Döhle bodies. This pattern of coarse, persistent granulation with otherwise normal cell morphology is characteristic of the Alder–Reilly anomaly, helping to distinguish the finding from toxic granulation [1][2][3].
The presence of these inclusions across several white cell lineages, neutrophils, lymphocytes, and monocytes, is an important morphological clue. Unlike reactive changes, which are temporary and limited to neutrophils, Alder-Reilly anomaly represents a stable, inherited pattern of abnormal granulation that remains consistent over time. The granules correspond to abnormal primary lysosomes filled with partially degraded mucopolysaccharides. Their dense staining and coarse texture reflect the accumulation of storage material rather than a response to infection or inflammation. In well-prepared smears, the inclusions are visible even at low magnification and retain a deep violet color at higher magnification, making digital morphology platforms such as CellaVision particularly effective for both identification and teaching [2][4][5].
While the Alder-Reilly anomaly is a striking hematological finding, it is not a disease in itself but rather a morphological manifestation of an underlying inherited metabolic disorder, most commonly one of the mucopolysaccharidoses (MPS). These lysosomal storage disorders result from deficient degradation of glycosaminoglycans, leading to their accumulation within various tissues. Clinically, affected individuals may present with coarse facial features, skeletal deformities (dysostosis multiplex), joint stiffness, development delay, hepatosplenomegaly, and recurrent respiratory infections. The hematologic findings thus server as an important diagnostic clue that can support recognition of these systemic conditions when correlated with clinical and biochemical data. [2][5]
Recognizing this distinctive appearance, especially when found in both granulocytes and lymphocytes, should prompt consideration of an underlying mucopolysaccharidosis manifesting with Alder-Reilly-type inclusions. Although the morphological changes are striking, the leukocytes generally function normally. Correct morphological interpretation therefore provides diagnostic insight rather than prognostic information, emphasizing the continuing importance of visual morphology and digital microscopy in modern hematology [1][2].
Reference:
[1] Bain BJ. Blood Cells: A Practical Guide. 6th ed. Hoboken (NJ): Wiley-Blackwell; 2024.
[2] World Health Organization. Classification of Tumours of Haematolymphoid Tissues. 5th ed. Lyon: IARC; 2024.
[3] To M, Villatoro V. Alder-Reilly Anomaly. In: A Laboratory Guide to Clinical Hematology. LibreTexts; 2020.
[4] Do L, Pasalic L. Lymphocytes in Sanfilippo syndrome display characteristic Alder-Reilly anomaly. Blood. 2019;134(14):1194.
[5] Jain R, Khurana U, Bhan BD, Goel G, Kapoor N. Mucopolysaccharidosis: a case report highlighting hematological aspects of the disease. J Lab Physicians. 2019;11(1):97–99.