Patient case #8 - Mantle Cell Lymphoma
Description
A man in his early 70s came to the emergency room with abdominal pain, loss of appetite, fever, night sweats, swollen lymph nodes in the neck, enlarged spleen and liver and back pain.
He was immediately hospitalized, and blood samples were drawn.
CBC results:
| Test | Results | Unit |
|---|---|---|
| WBC | 75 | x109/L |
| HGB | 75 | g/dL |
| MCV | 99 | fL |
| PLT | 103 | x109/L |
The CBC results were flagged with Blasts/Abn Lympho which triggered analysis on Cellavision DC-1.
The cell counter flagged for Blast/Abnormal Lymphocytes. A blood smear was made and scanned on a CellaVision® DC-1 analyzer.
Smear analysis on CellaVision® DC-1:
| WBC differential | % | x109/L |
|---|---|---|
| Band neutrophils | 0,9 | 0,7 |
| Neutrophils | 8,1 | 6,1 |
| Eosinophils | 0,9 | 0,7 |
| Lymphocytes | 6,3 | 4,7 |
| Monocytes | 0,9 | 0,7 |
| Abnormal lymphocytes | 82,9 | 62,2 |
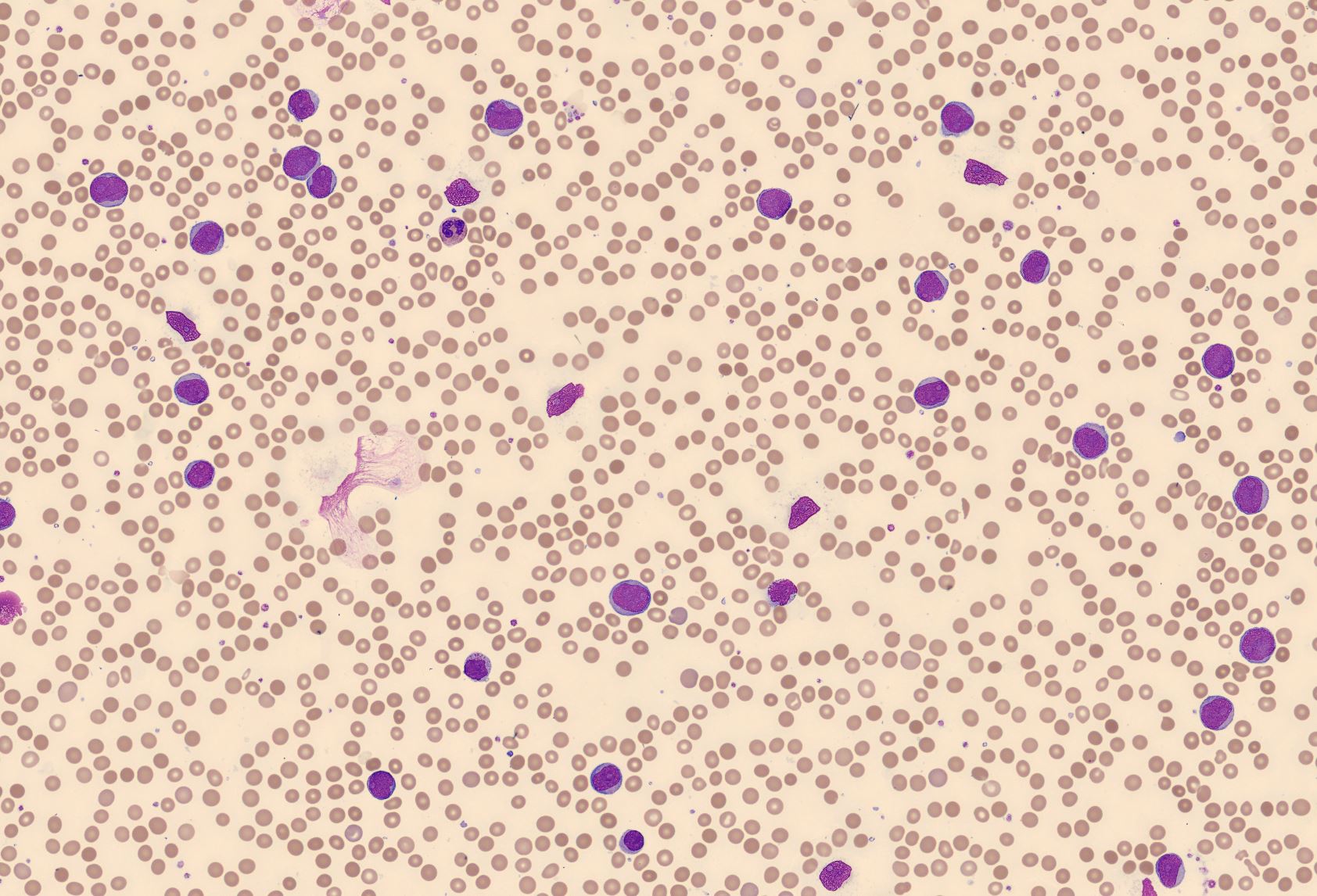
The MedTech could immediately see that something was seriously wrong.
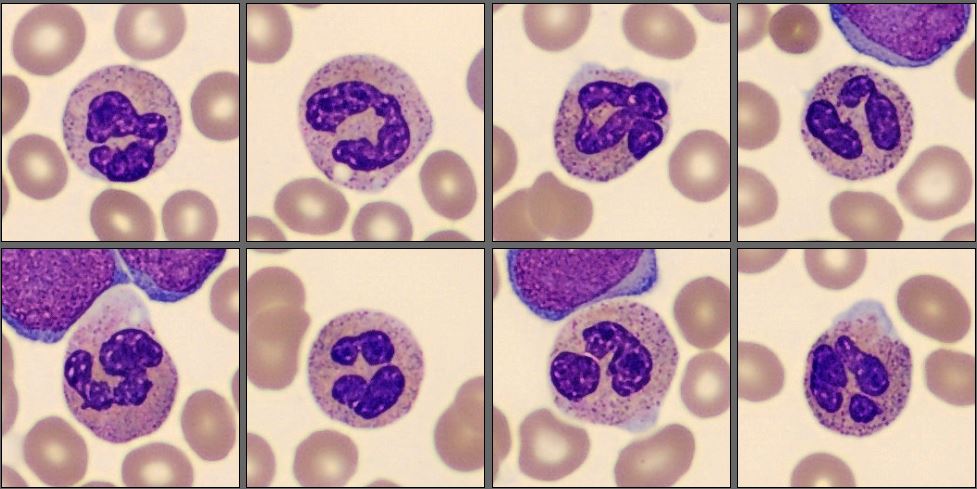
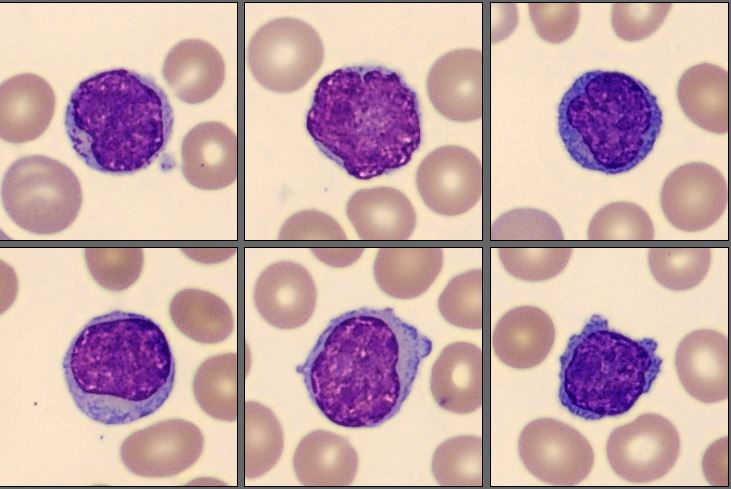
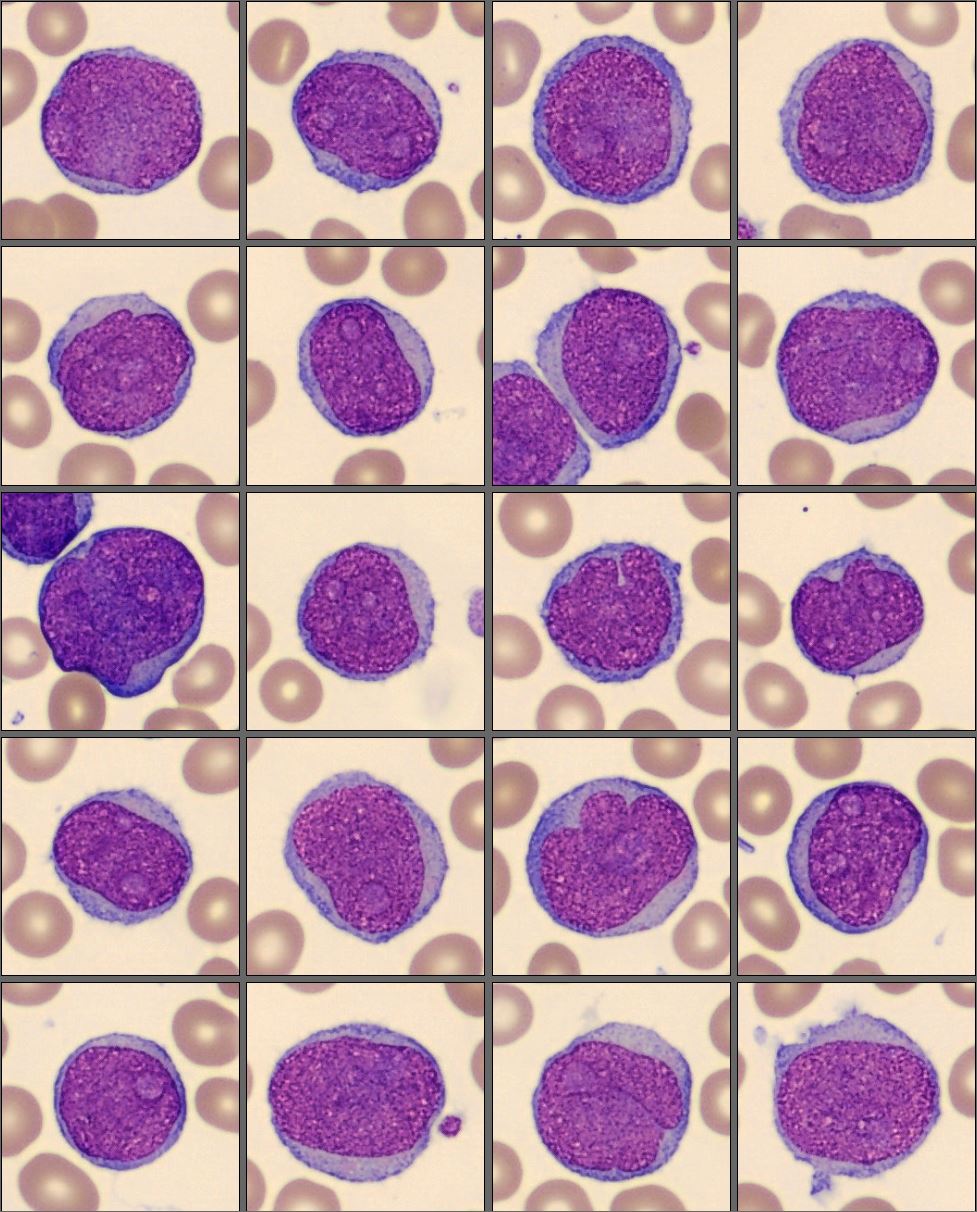
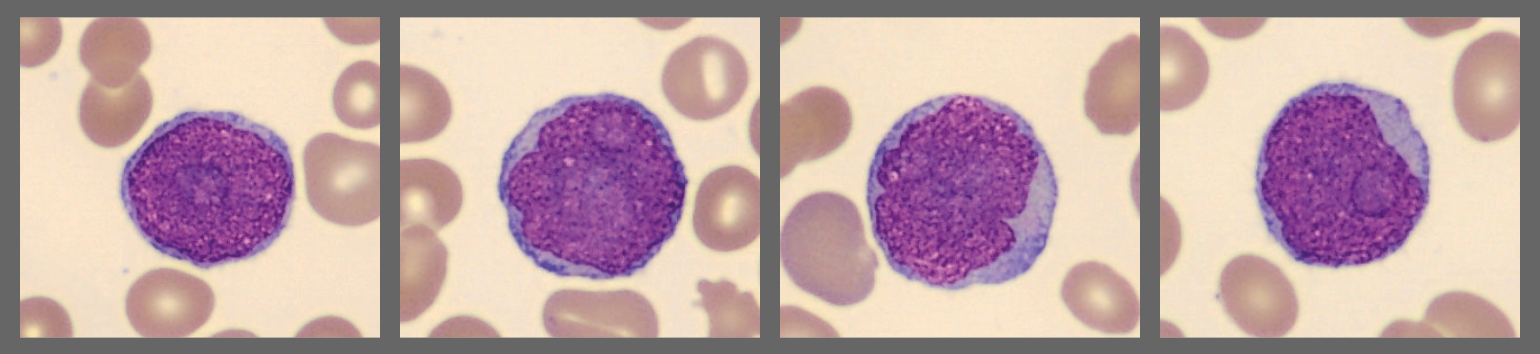
On the CellaVision® Remote Review Software, the MedTech could confirm that the number of neutrophils and lymphocytes were low. A big population with medium-sized to large blast-like cells with somewhat pleomorphic nucleus, stippled chromatin and with one or more clearly visible large nucleoli where seen. These cells were preclassified by the CellaVision® Peripheral Blood Application as Blasts but were reclassified by the MedTech to Abnormal lymphocytes. The differential was sent to a hematopathologist for consultation.
Diagnosis
Non-Hodgkin Lymphoma, Mantle Cell Lymphoma
Flow cytometry data: Lambda Restricted Cells, CD5+, CD19+ bright CD20, CD22+, variable CD38, CD71+, HLA-DR+, CD10-, CD34-
Discussion
Mantel cell lymphoma (MCL) is a rare and aggressive form of a B- cell, non-Hodgkin lymphoma (NHL). It derives from the mantle zone of lymphoid follicles. The mantle zone is a part of the secondary lymphoid nodule and surrounds the central germinal center and normally contains small mature B-lymphocytes. [1][2]
MCL accounts for 3-10% of B-cell lymphomas world-wide. The median age is 68-69 years, and it is more common in the male population. [1]
It is not known what exactly causes MCL, but about 85% of the diagnosed patients have a translocation between chromosomes 11 and 14. [1][3] MCL expresses pan-B-cell markers – CD19, CD20, CD22 and CD79a. CD5, FMC7 and CD43 are usually positive, while CD10 or BCL6 is often negative but can be positive in aggressive variants. [1]
MCL usually involves the lymph nodes, but also the gastrointestinal tract, spleen, bone marrow and Waldeyer ring (tonsillar ring [4]). Other organs that can be involved include the skin, the endocrine glands, lungs, and CNS, but these are more common with relapse disease. [1]
In many patients, we will not see any abnormalities in the peripheral blood. The disease can go into a leukemic phase where the lymphoma cells will be found in the blood. The cells often vary from small to medium size to large. They are often pleomorphic – irregular, angular with clefted nuclei, and they often have prominent nucleoli. The bone marrow is infiltrated in most of the diagnosed patients. [5]
An experienced hematopathologist/MedTech can determine whether the MCL is the common type or a rarer blastoid variant, where the cells are bigger and grow more rapidly. This type is more aggressive and harder to treat. This blastoid variant may be present at diagnosis or emerge over time. [3]
MCL used to be considered as incurable, but with new therapeutic approaches the median overall survival time has increased from 3 years to 5-10 years. Evaluation of a variety of different prognostic markers for conventional MCL has been done, and in the future with new treatments some patients may potentially be cured. [1]
___
Reference:
[1] Klapper, W., Ferry. JA., Hermine. O., Li, S., Lossos. IS., Medeiros LJ., Naresh. KN., Rosenquist. R., Rule. S., Stilgenbauer. S. Mantle cell lymphoma. In: WHO Classification of Tumors series, 5th ed.; vol 11, IARC publications, 2024. p. 446-452.
[2] Standring, S. Gray's Anatomy: The Anatomical Basis of Clinical Practice. Gray's Anatomy Series: Elsevier Limited, 2016
[3] O’Connor, O.A. The Leukemia & Lymphoma Society, (2014) Mantle Cell Lymphoma Facts
[4] NIH, National Cancer Institute, NCI's Dictionary of Cancer Terms
[5] Bain. B.J., Clark. D.M., Wilkins. B.S. Bone Marrow Pathology, 4th ed, Wiley-Blackwell, ISBN 978-1-4051-6825-0. 2010, p. 338-342.