Monthly Cell Challenge #2 / 2025

Child with atypical white blood cell granulation
Description:
A pediatric patient with albinism and a history of upper respiratory infection, an ear infection, and bruising arrived at their pediatrician for an examination. Upon neurological exam, the patient was experiencing nystagmus (rapid, uncontrollable eye movements).
CBC results:
| Test | Result | Units |
| WBC | 4.9 | x109/L |
| Hemoglobin | 15.2 | g/dL |
| PLT | 235 | x109/L |
Peripheral Blood smear analysis on CellaVision® DC-1
| WBC Differential | % | x109/L |
| Neutrophils | 44.0 | 2.2 |
| Eosinophils | 1,0 | 0 |
| Basophils | 1,0 | 0 |
| Lymphocytes | 33 | 1.6 |
| Monocytes | 11,0 | 0.5 |
| Reactive lymphocytes | 10,0 | 0.5 |
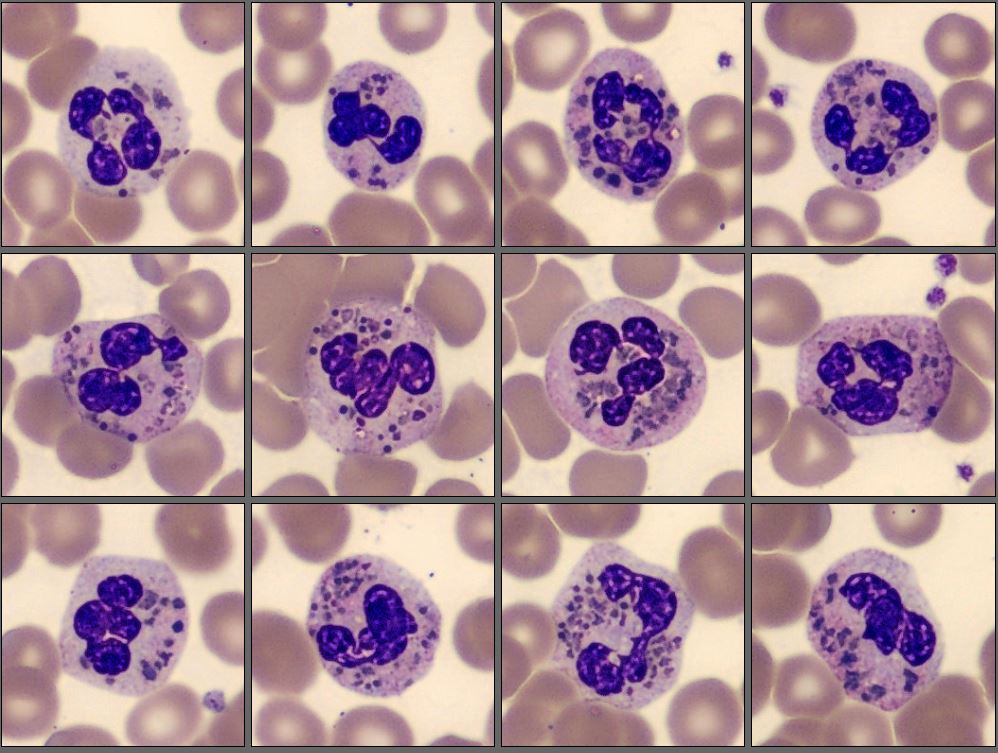
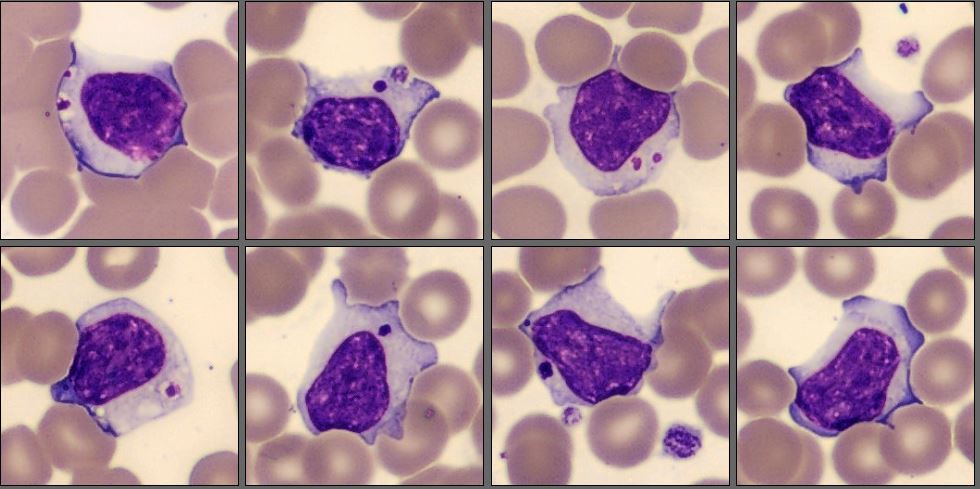
CellaVision showed large, abnormal granules in the granulocytes which did not look like toxic granulation in the neutrophils. The reactive lymphocytes exhibit large azurophilic granules.
Diagnosis:
The patient was diagnosed with Chediak-Higashi syndrome. A genetic test showed 1q42.1-q42.2, LYST Gene Mutation.
The presence of abnormally large granules seen in the CellaVision® Review Software is diagnostic and was confirmed with genetic test for the LYST mutations.
Discussion:
Chediak-Higashi syndrome is a rare, autosomal recessive condition that involves phagocytic cell defects. It is usually found early in life and is characterized by oculocutaneous albinism, frequent respiratory and other infections, bruising, and so on. Some individuals may also develop neurological symptoms. The cells containing these abnormal granules function poorly and their phagocytic function is reduced.
Morbidity in patients with Chediak-Higashi syndrome is a result of recurrent infections or development of an accelerated phase. This accelerated phase will cause, for instance, fever, lymphoproliferation into major organs, and neurologic changes. Eighty percent of the deaths occur in the first decade of life, and those who survive into adulthood develop progressive neurological symptoms.
The only way to treat Chediak-Higashi syndrome is with allogeneic hematopoietic stem cell transplantation (HSCT). HSCT should be done as soon as the diagnosis is established. The transplant will, however, only cure the hematological and immune dysfunction and will not stop the progressive neurological impairment.
The syndrome is caused by a mutation in the LYST (lysosomal trafficking regulator) gene. This gene is responsible for the regulation of lysosomal trafficking and the synthesis, fusion, and transport of cytoplasmic granules.
Reference:
Curr Opin Hematol. 2023 Apr 25;30(4):144–151. doi: 10.1097/MOH.0000000000000766 - Chediak-Higashi Syndrome - Mackenzie L Talbert 1, May Christine V Malicdan 1,2,3, Wendy J Introne 1,3