Patient case #4 - Plasma cell leukemia

Description
A 68-year-old female with a history of breast cancer presented with cough, fever, chills, shortness of breath, weakness, and unexplained weight loss.
CBC results:
| Test | Result | Units |
|---|---|---|
| WBC | 27.7 | x109/L |
| HGB | 9.0 | g/dL |
| MCV | 81.9 | fL |
| PLT | 105 | x109/L |
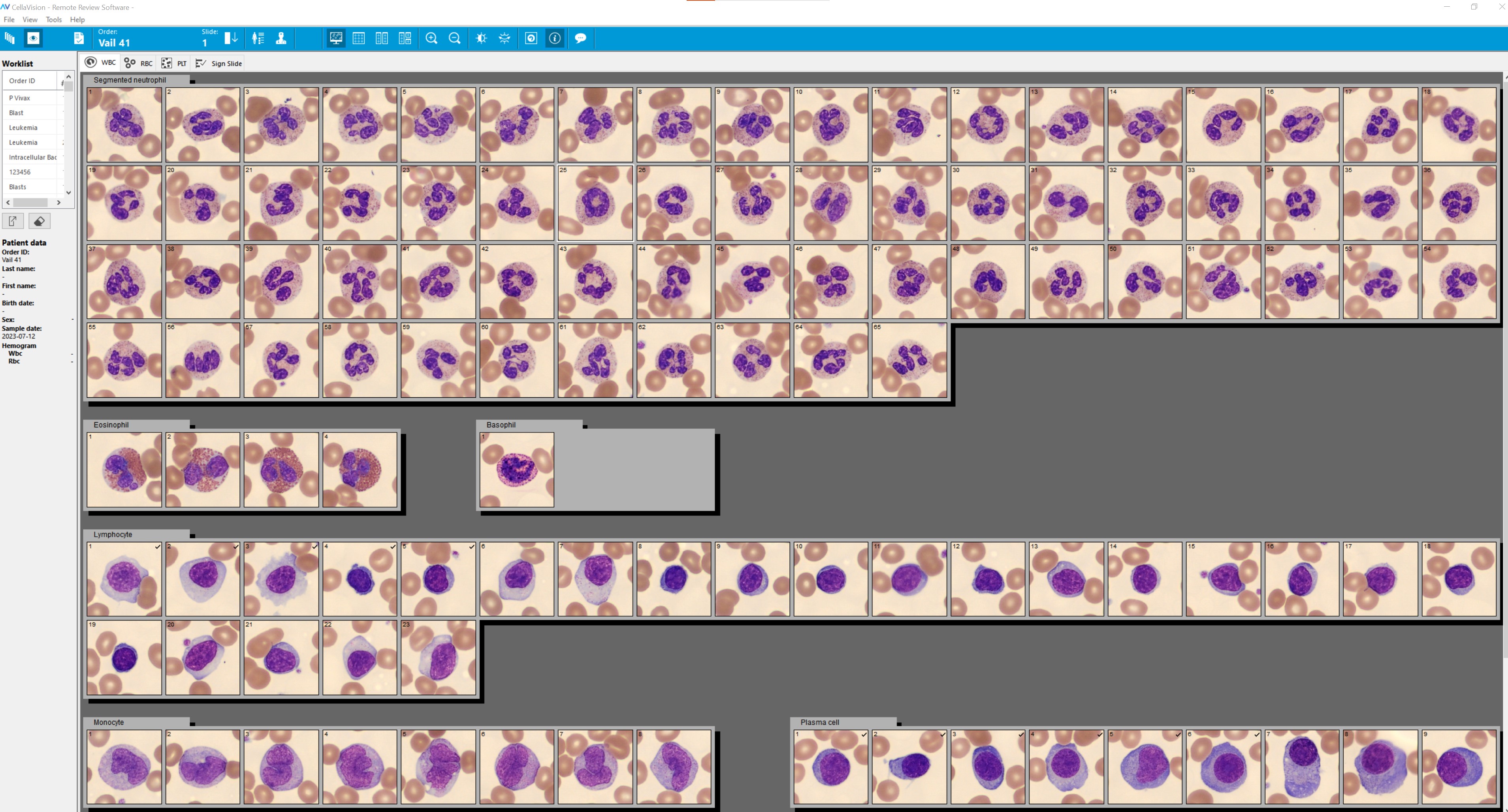
The automated differential was flagged with Blasts/Abn Lympho. A blood film was prepared, stained with Wright-Giemsa, and analyzed on CellaVision DC-1.
The DC-1 results are below (normal and reactive lymphocytes combined):
|
Cell Class |
% |
x109/L |
|---|---|---|
| Segmented neutrophils |
59 |
16.3 |
| Lymphocytes |
18 |
5.0 |
| Monocytes |
7 |
1.9 |
| Eosinophils |
4 |
1.1 |
| Basophils |
1 |
0.3 |
| Variant (reactive) lymphocytes |
3 |
0.8 |
| Plasma cells |
8 |
2.2 |
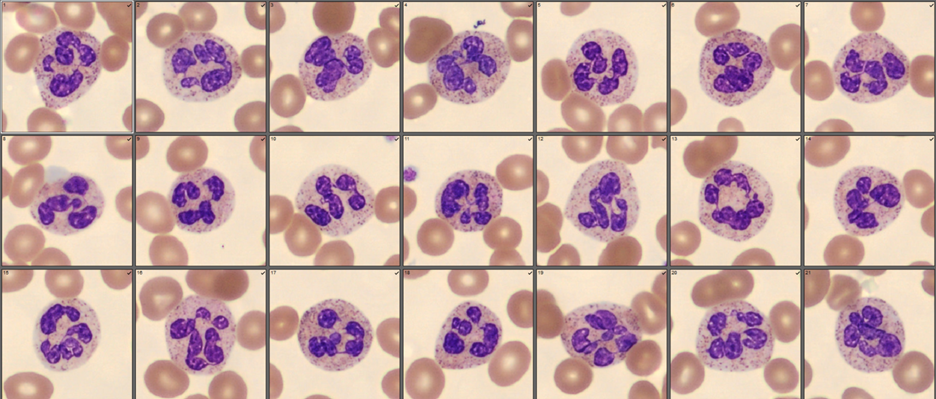
Hypersegmented neutrophils were found:
Plasma cells, some with immature features could not be clearly distinguished from normal and reactive lymphocytes. A side-by-side view was used to identify the plasma cells (lymphocytes on the left, plasma cells on the right):
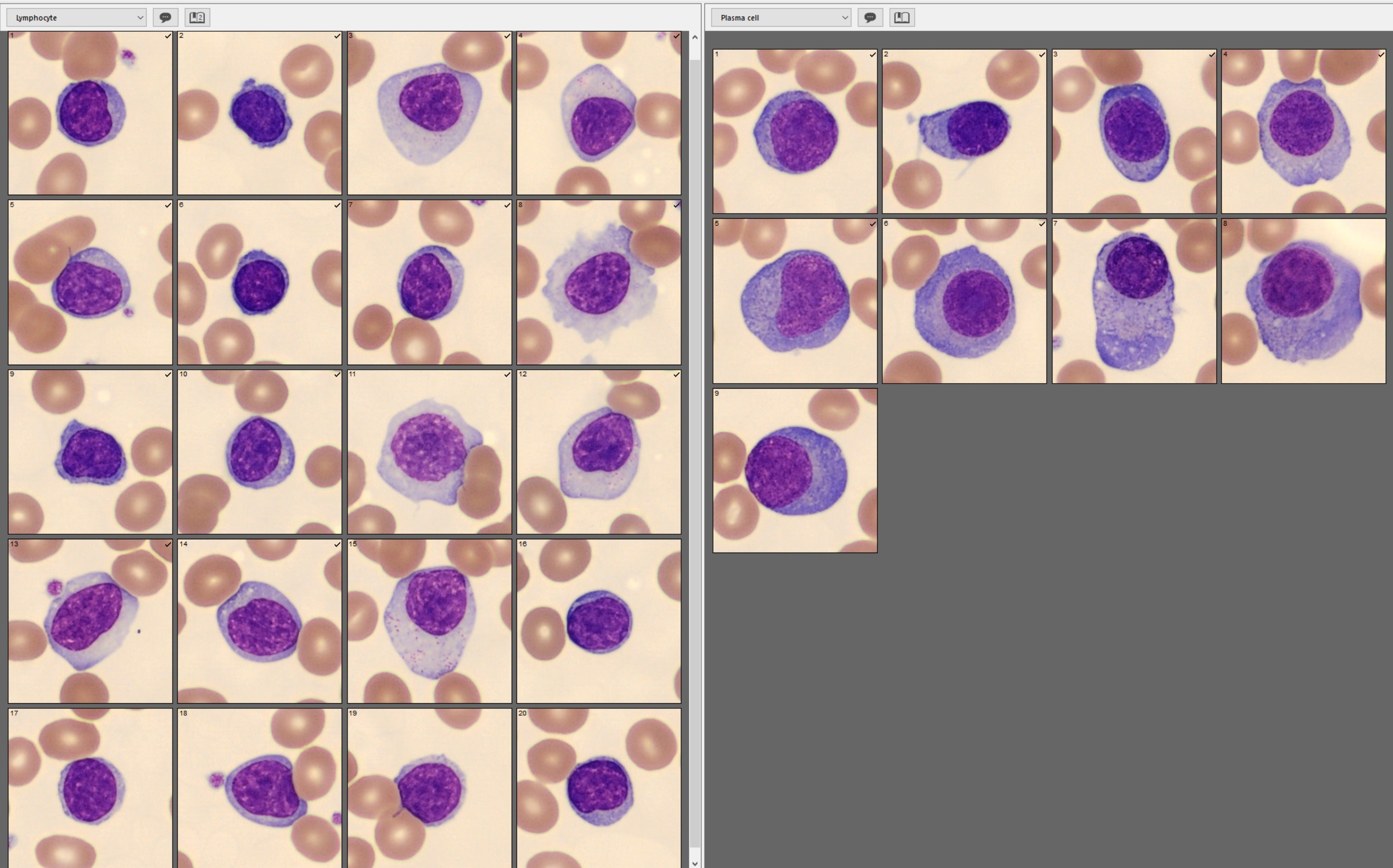
Morphological characteristics helpful in differentiating lymphocytes and plasma cells:
|
|
Lymphocytes |
Plasma cells |
|---|---|---|
| Chromatin pattern | Mature, irregularly clumped with visible pale white spaces |
Immature, smooth |
| Cytoplasm color | Light blue | Darker shade of blue |
| Perinuclear halo/visible golgi | Not visible | Visible |
| Nuclear shape | Irregular | Regular, round-oval |
Serum protein electrophoresis and immunofixation revealed a monoclonal protein (M-spike), IgG kappa
Plasma cell immunophenotype by flow cytometry:
- CD38+, CD138+, dim CD56+, kappa light chains positive
- CD9-, CD10-, CD71-, CD117-, HLA-DR-, lambda light chains negative
Diagnosis/Summary:
Diagnosis: Primary plasma cell leukemia (PCL).
PCL is a rare and aggressive malignancy of plasma cells that presents in the peripheral blood. Primary PCL occurs with no history of multiple myeloma (MM), whereas secondary PCL is a form of end-stage MM. The prognosis is dismal. Overall survival is approximately one year in primary PCL and one month in secondary PCL.
The diagnosis of PCL is based on > 5% plasma cells on the blood film 1 with confirmation of clonality. In this case, the plasma cells were kappa light chain positive and lambda light chain negative, indicating monoclonality.
Morphology can vary in PCL, resulting in potential errors in the WBC differential results. Immature/abnormal plasma cells can resemble normal lymphocytes, reactive lymphocytes, abnormal lymphocytes, or blasts, as shown below:
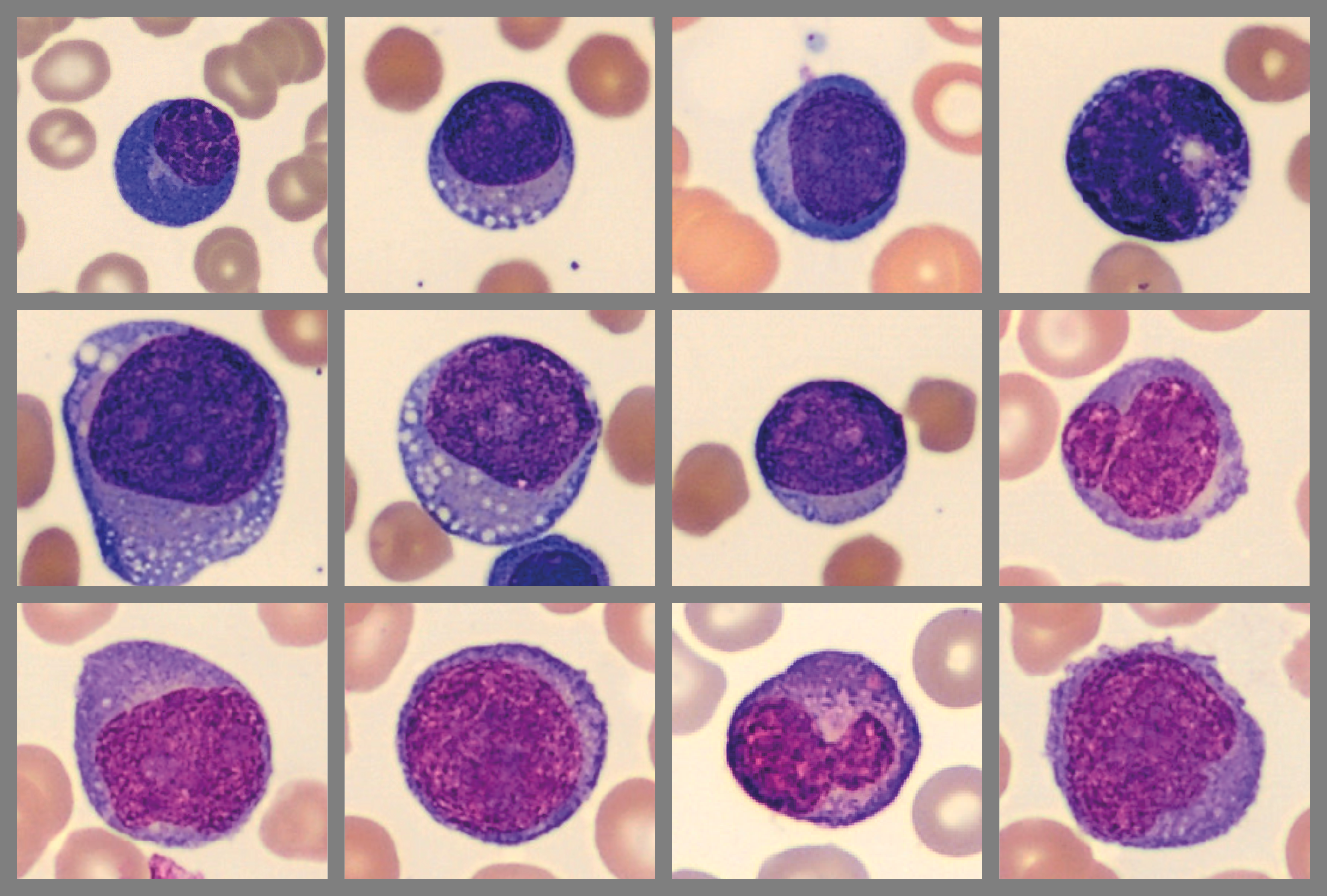
Blood films containing immature/abnormal plasma cells will often reveal at least a few identifiable plasma cells. This should increase suspicion and trigger a search for other cells with less recognizable characteristics. If present, a close examination should uncover a continuum of morphological features in the entire plasma cell population.
Circulating polyclonal plasma cells can be seen in various benign conditions. Morphology alone cannot reliably differentiate these cells from monoclonal plasma cells. Additional testing is required.
A correct and timely diagnosis of PCL is important because patients need to begin treatment as soon as possible. An accurate diagnosis depends on the ability to identify all types of plasma cells present during blood film review. The simultaneous comparison of different cell classes using digital morphology can assist in this process and help improve confidence in the reported results.
__
1. Fernández de Larrea C, Kyle R, Rosiñol L, et al. Primary plasma cell leukemia: consensus definition by the International Myeloma Working Group according to peripheral blood plasma cell percentage. Blood cancer journal (New York). 2021;11(12):192-192.